Nephrology
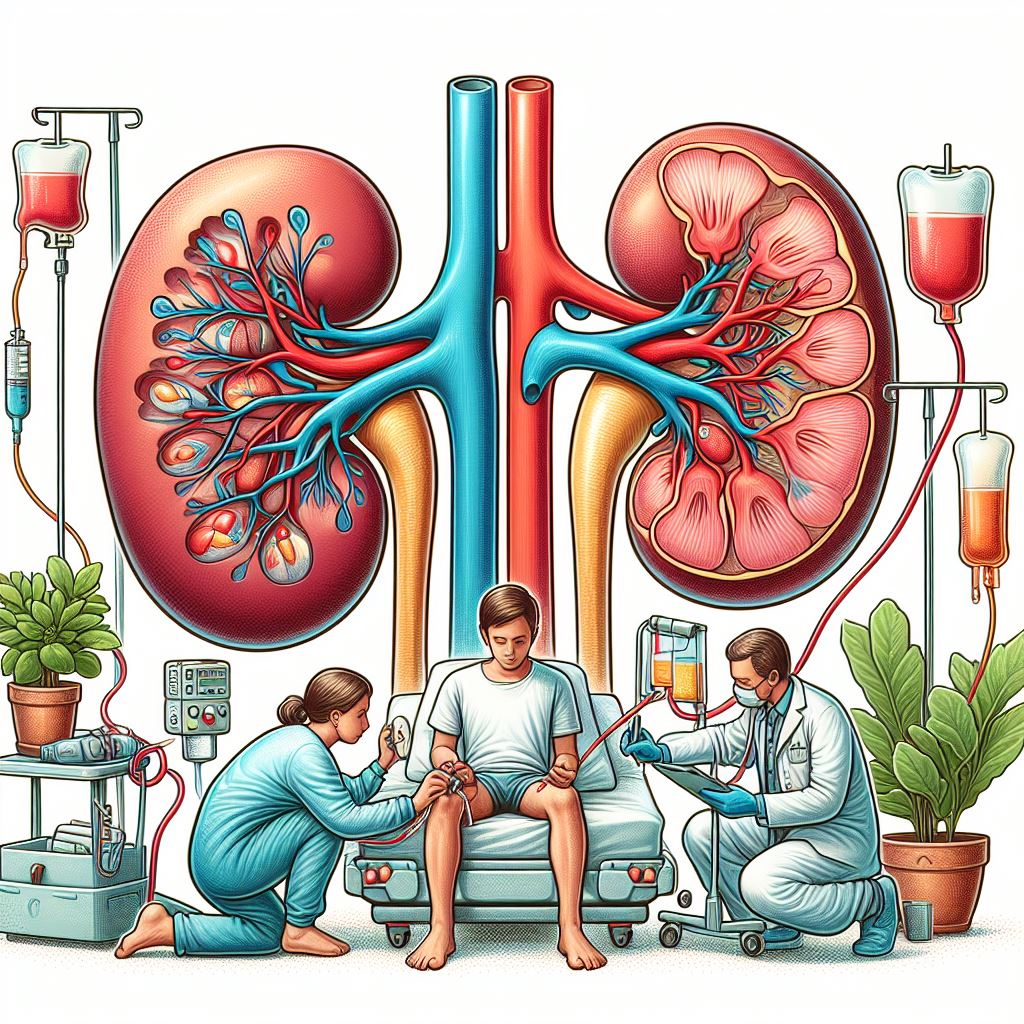
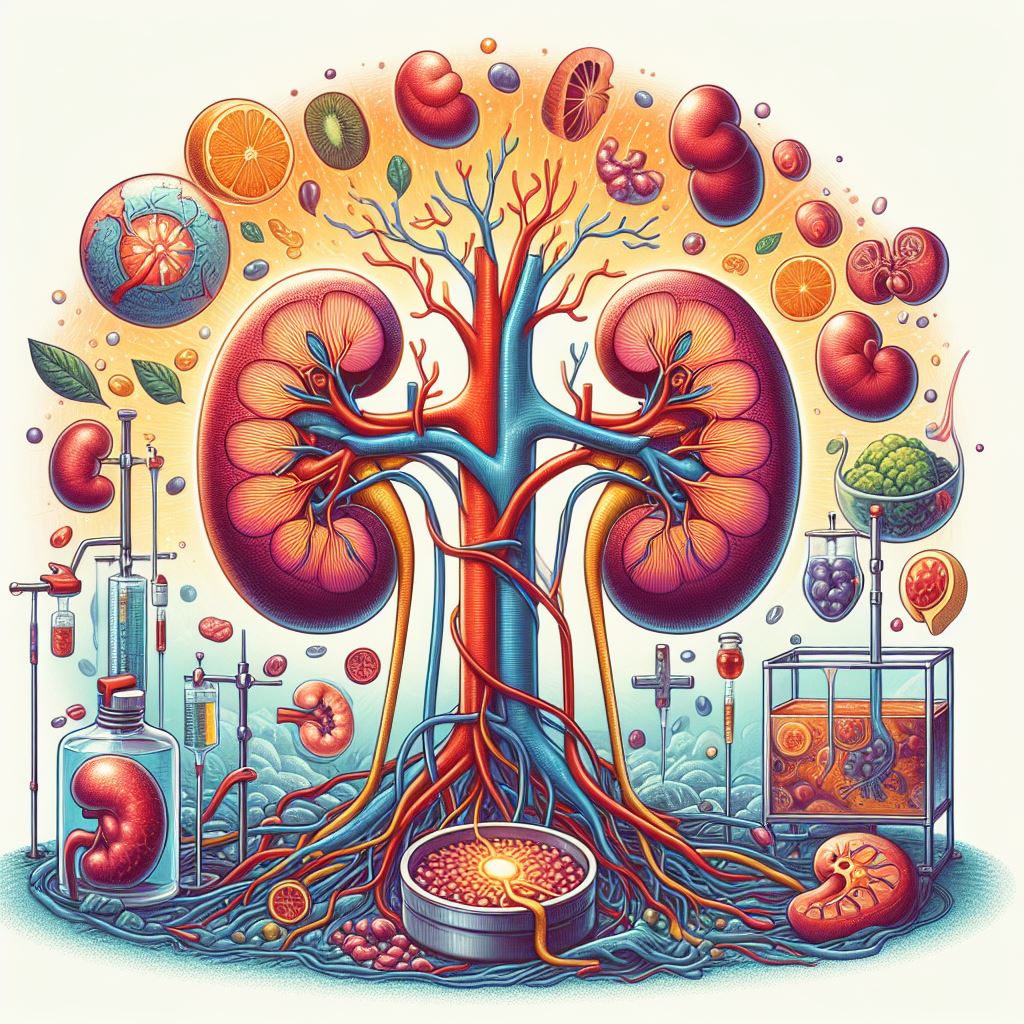
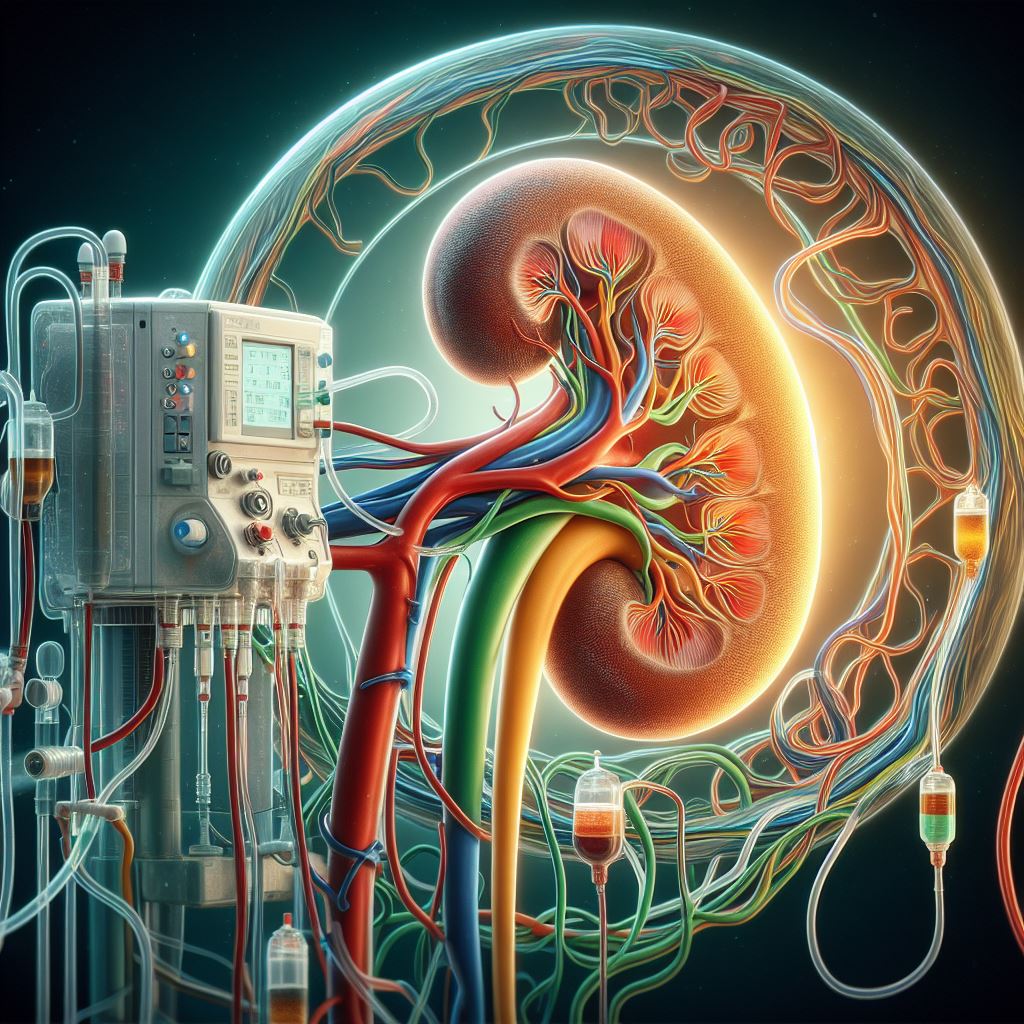
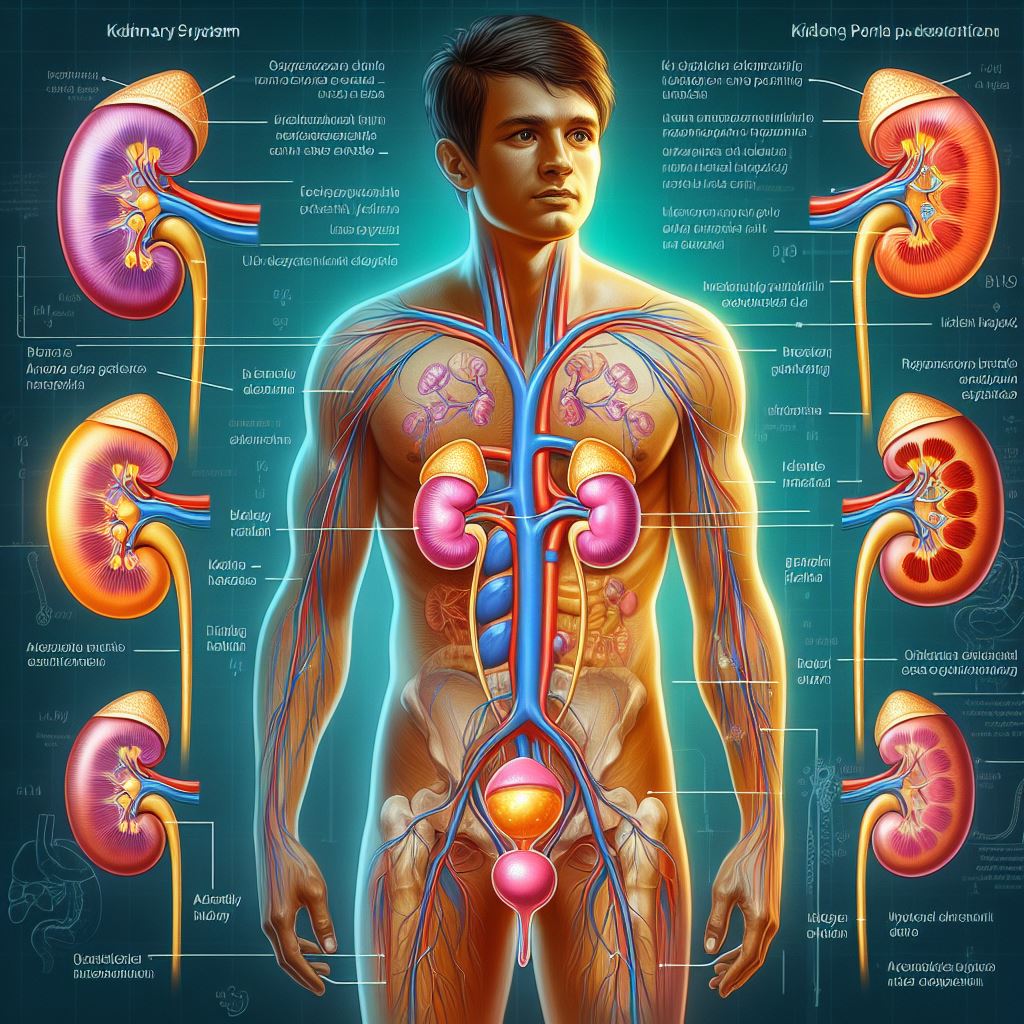
Nephrology is an essential medical specialty that deals with the kidneys, which are crucial organs responsible for various vital functions in the human body. The kidneys perform a wide range of tasks, including keeping fluid balance, filtering waste products and excess substances from the bloodstream, regulating blood pressure, and producing hormones involved in red blood cell production and bone health.
As experts in kidney health, nephrologists oversee diagnosing, treating, and managing an array of kidney-related conditions and disorders. These include:
- Chronic kidney disease (CKD): This progressive condition occurs when the kidneys lose their ability to function effectively over an extended period. CKD can result from several factors, such as diabetes, hypertension, autoimmune diseases, or genetic conditions. As the disease progresses, patients may need dialysis or a kidney transplant.
- Acute kidney injury (AKI): Unlike CKD, AKI is a sudden and temporary loss of kidney function. It can occur due to factors like severe infections, toxic substances, dehydration, or reduced blood flow to the kidneys. Timely intervention is essential to prevent permanent damage or the progression to chronic kidney disease.
- Glomerular diseases, Glomerulonephritis (GN): Glomeruli, the kidney's tiny filtering units, can be affected by various diseases, such as glomerulonephritis or diabetic nephropathy. These conditions can cause inflammation, scarring, and damage to the kidneys, impairing their ability to filter waste and keep fluid balance.
- Kidney stones: These are solid deposits of minerals and salts that form within the kidneys. They can cause intense pain, infection, and obstruct urine flow. Nephrologists can help manage kidney stones through medication, lifestyle changes, or minimally invasive procedures.
- Tubular disorders: The renal tubules manage reabsorbing essential substances and secreting waste products. Conditions like renal tubular acidosis or Fanconi syndrome affect the tubules' proper functioning, leading to electrolyte imbalances and other complications.
- Renal artery stenosis: This condition occurs when the renal arteries, which supply blood to the kidneys, become narrowed due to plaque build-up or other factors. Reduced blood flow can impair kidney function and contribute to high blood pressure.
- Polycystic kidney disease (PKD): A genetic disorder characterized by the growth of numerous cysts in the kidneys, leading to reduced kidney function and eventual kidney failure.
- Electrolyte imbalances: Abnormal levels of essential electrolytes in the body, such as sodium, potassium, and calcium, which can be caused by kidney dysfunction.
- Hypertension (high blood pressure): Elevated blood pressure that can damage the blood vessels in the kidneys and impair kidney function.
- Kidney infections: Infections like pyelonephritis result from bacteria entering the kidneys, usually from the urinary tract. Symptoms may include fever, back pain, and frequent urination. Antibiotics and other treatments are essential to prevent complications.
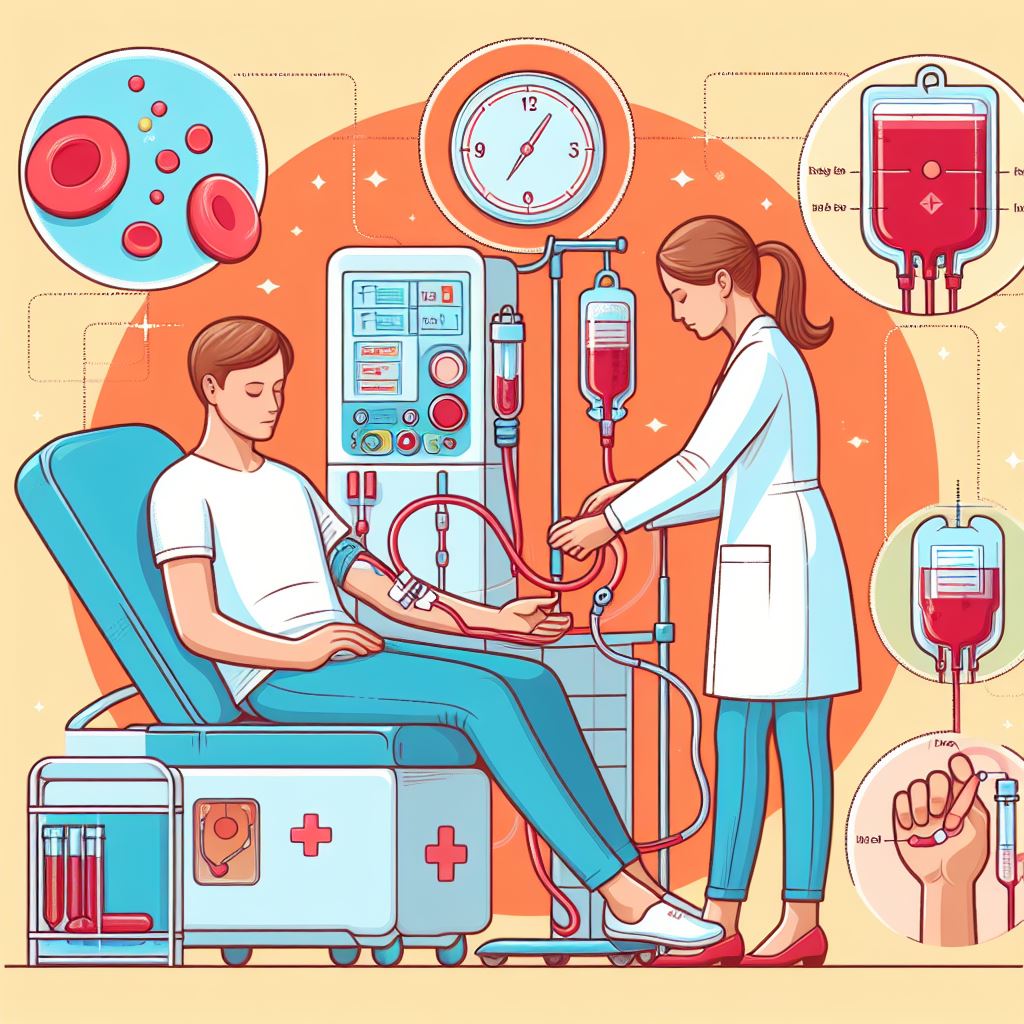
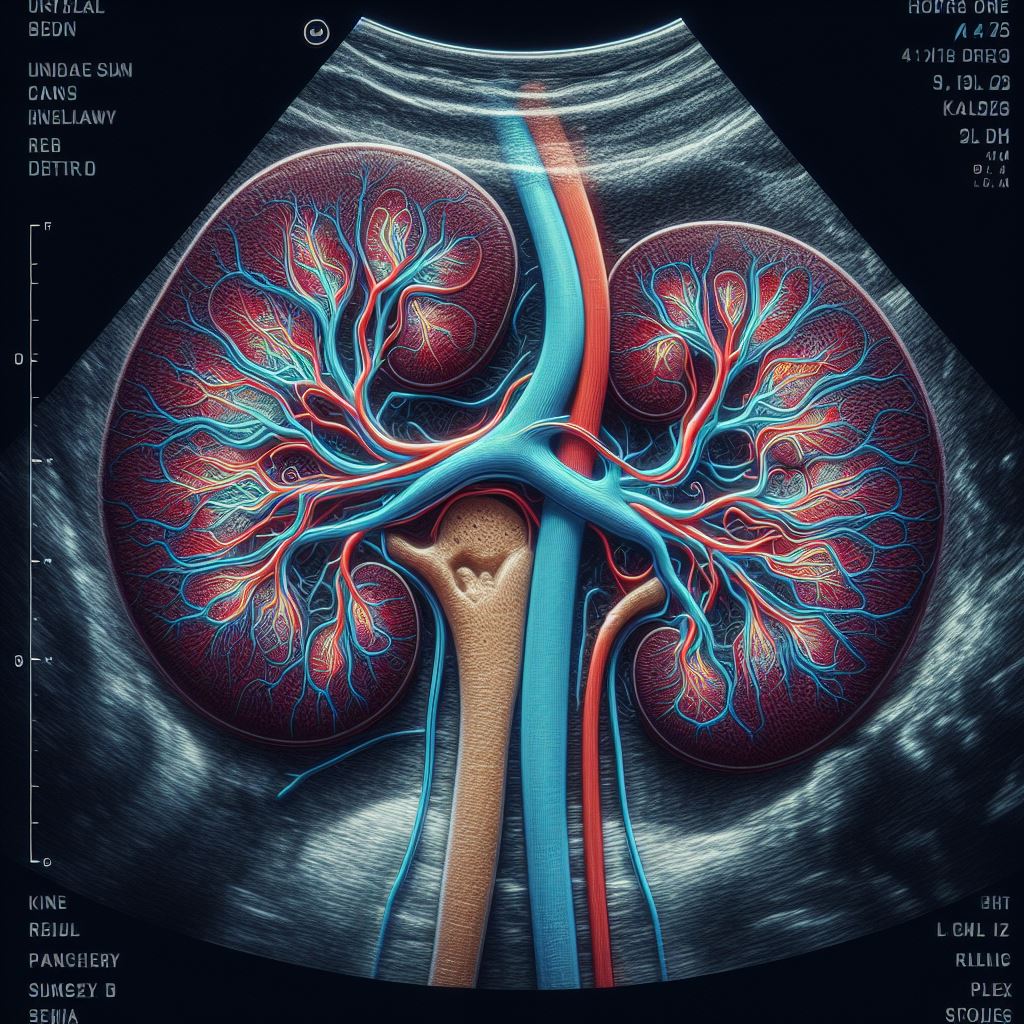
Nephrologists employ various diagnostic tools and tests to evaluate kidney function, including blood tests, urine tests, imaging studies (e.g., ultrasound, CT scans), and kidney biopsies. They supply tailored treatment plans for each patient, which may involve medications, dietary modifications, lifestyle changes, or medical procedures like dialysis and kidney transplantation.
In summary, nephrology is a vital medical specialty that deals with the diagnosis, treatment, and management of kidney-related conditions. Nephrologists play a crucial role in supporting kidney health and helping patients manage their conditions to improve their overall quality of life.